|
 |
We begin by reviewing the list on the Scratch Pad to identify hospital-acquired respiratory viral infections (RV HAI or HCAI).
Just so that we are clear, we wrote:
“RV HAIs are associated with longer hospital stays and higher ICU admission rates. In a cohort of 1,700 patients with RV HAI, patients had longer mean lengths of stay (e.g., 21 days vs. 5 days in community-acquired cases). These patients were older, had pre-existing respiratory disorders or were immunosuppressed and faced greater RV HAI risk. They were also likely to exhibit typical respiratory infection symptoms, which could delay diagnosis.
RV HAIs are also associated with significantly higher mortality compared with community-acquired cases, often with several-fold greater risk. Among patients who acquired influenza in hospital, 21.7% died compared with 4% among patients with negative test results. So, roughly 1 in 5 hospital-acquired influenza patients die in hospital, compared with about 1 in 25 in similar hospitalised patients who do not acquire influenza. The odds of in-hospital death were significantly higher for those with HAI-influenza, even after adjusting for age and comorbidities.”
So in the TTE office, we tried to find some joined-up government programmes dealing with the problem through the eyes of two old geezers who’ve seen a few winters and too many “initiatives.” Joined-up government wouldn’t start with a press release, it’d start with the same set of numbers on everyone’s desk. All are looking at the same severity data, not each running their own pet dashboard and panicking on different days—the kind of system that works so smoothly, no one notices.
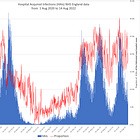
Just after the Covid era, we laboriously estimated the likely impact of COVID-19-associated HAIs in the UK; a conservative estimate was 40%. No one could tell us how many of these subsequently died in the hospital. Wales, Scotland and Northern Ireland provided us with data, assistance and clarification. NHS England, twisted, evaded, dodged and finally came up with the answer:
“We do not hold granular hospital admission data reported by days of positivity to SARS-CoV-2 since admission, or data going back to March 2020.”
They had no idea how many folks in England were admitted with a negative test, which subsequently turned positive after eight or more days in hospital - Our wildly optimistic timeline for capturing all RI HAIs.
Fast forward to the current automated electronic bulletins from public health bodies, and we still haven’t found evidence of a coordinated programme to address respiratory viral HAIs, despite the “Superflu” nonsense. Joined-up government wouldn’t be a shiny “zero tolerance” slogan. It’d be dull, practical, and agreed before the wards fill up.
Trying to find the joined-up government programs
We reviewed the websites of the three obvious candidates for tackling HAIs: DHSCS, Scare Agency, and NHS England.
Of these, the only credible source was the UKHSA’s page on HCAIs, published in July 2014 and last updated in September 2023.
The website is the usual government mess of information. Information posted in May 2025 has not been updated since 2023.
The point prevalence survey link dates back to 2016, even though the survey’s latest update states 2023. Despite this mess, we pressed on to find the 2023 publication
After locating the 2023 point-prevalence survey (PPS) on HCAIs, we searched the document and identified five hits for “virus”.
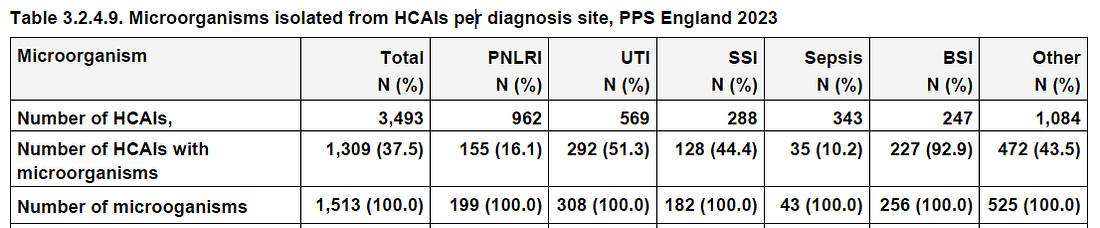
Table 3.2.4.9. Reports “Microorganisms isolated from HCAIs per diagnosis site, PPS England 2023” (see pdf page 40).
PNLRI stands for Pneumonia or lower respiratory tract infection, UTI is a urinary tract infection, SSI is a surgical site infection, and BSI is a Bloodstream infection.
Aside from its sell-by date, can you see anything unusual in the data?
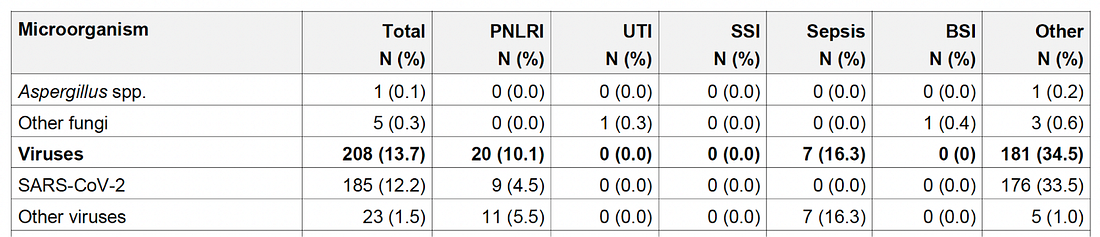
No? Then have a look at this screengrab from pdf page 42:
Viruses account for 13.7% of HAIs, primarily due to SARS-CoV-2, and only 10% of PNLRI.
Given the number and fuss around “superflu” and annual hospitalisations, panic, fear, etc., we are unable to understand how many HAIs are caused by respiratory viruses, regardless of agent and how many end in deaths,
We also can’t tell if any of them are investigated, and how it is possible that only 13.7% of HAIs in 2023 involved viruses (mostly Covid), with a small proportion not investigated? We also don’t know how many of these were co-infections with other viruses or with superimposed bacterial pneumonia in a selected population highly vulnerable to these pathogens.
From this 2023 report, you can see the dead hand of the NHS bureaucracy. Concentration on bacteria (Klebsiella, Pseudomonas, etc.). It ignores the worst-case killers, which MSM, Ministers, authoritarians, modellers and charlatans united indicated as the winter devil.
We did not want to jump to conclusions, so before Christmas, we submitted FOI requests to UKHSA, DHSC, and NHSE.
We fired them off to all three at the same time to avoid the “pass the parcel” game we have been frequently subjected to (“we do not deal with HAIs ask the other bodies”). They’d look pretty silly if they all answered this at the same time, would they not?
Our requests to all three bodies were 100% identical:
Subject: Programme for VIRAL RESPIRATORY hospital-acquired infections
Do you have a programme or standard operating procedure to identify and minimise the consequences of VIRAL RESPIRATORY hospital-acquired infections (HCAIs)?
If so, can you point me to it, please?
If so, do you have a programme or standard operating procedure to identify and minimise the consequences of INFLUENZA hospital-acquired infections (HCAIs)? If so, can you point me to it, please?
If so, do you have a programme or standard operating procedure to identify and minimise the consequences of SARS-CoV-2 hospital-acquired infections (HCAIs)? If so, can you point me to it, please?
We await the evasions, body swerves, boilerplate, and patronisation answers. As to the joined-up programs, we are none the wiser.
This post was written by two old geezers who do not like “pass the parcel” and are beginning to understand why governments rely on modellers.